Hallticket no...1701006097
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan
71 YEARS OLD MALE WITH BREATHLESSNESS AND COUGH
CASE HISTORY:
71 years old male who is mason by occupation came to the hospital on 1st June 2022(1/06/22) with chief complaints
- breathlessness since 20days
-cough since 20days
-fever since 4 days
Daily routine of the patient :
He is Mason by occupation since 30 years.Daily he used to wake up at 6:30 am and goes to work by 9 am and return home by 5 pm.He doesn't wear mask while working.He sleeps at 10 pm.
History of presenting illness:
Patient was apparently asymptotic 2months back then he developed breathlessness of grade-1 (MMRC) , insidious in onset & progressive type and cough (dry) for which he visited govt hospital and received medications , during this time the symptoms are on& off
From past 20days —
**Breathlessness aggravated to grade 2 to 3
Aggravated on exertion
Relieved on rest
Associated with wheezing
No orthopnea and PND
**he developed cough with expectoration
Mucoid in consistency
Non foul smelling
Non blood stained
Aggravated during night time
** fever since 4days
which is low grade ,continuous in nature
Not associated with chills and rigors
Evening rise of temperature is present
Relieved on medications
History of past illness -
No history of similar complaints in the past
No history of TB , COVID 19 in the past
Not a known of diabetes , hypertension , CAD ,epilepsy
Personal history-
Diet-Mixed
Appetite -decreased
Sleep-adequate
Bowel movements-regular
Bladder movements-decreased flow of urine since 15days , associated with burning sensation
Addictions- smoking since 3years , 4 beedis per day
Alcohol -toddy , 1bottle from age of 22years
Stopped smoking and alcohol from 2months
Family history —
No similar complaints in the family
No history of TB , diabetes, hypertension, cad,epilepsy
General examination-
Patient is conscious ,coherent , cooperative
Thin built & moderately nourished
Vitals—
Temparature- 99 F
Pulse rate- 85 beats per minute
Respiratory rate- 20 cycles per minute
Blood pressure-120/80 mm Hg
Sp02-95% on room air
GRBS- 108 mg/dl
Pallor - absent
Icterus-absent
Clubbing-absent
Cyanosis -absent
Lymphadopathy- absent
Edema-absent
Systemic examination—
Respiratory system:
Inspection-
.Shape of chest-bilaterally symmetrical,elliptical
.Trachea- shift to right side
.Chest movements-decreased on right side
.No kyphosis and scoliosis
.No crowding of ribs
.No scars,sinuses,visible pulsations,engorged veins
.No drooping down of shoulders
.No supraclavicular and infraclavicular hollowing
.No intercoastal indrawing
Palpation-
.All inspectors findings are confirmed
.No local rise of temperature and tenderness
.Trachea-shift to right side
.Chest movements- decreased on right side
.Chest expansion-decreased on right side
.AP diameter-23 cm
.Transverse diameter-30cm
.hemithorax diameter on right side is less than that on left side
. Vocal Fremitus reduced on apical part of right side of chest
Percussion-
.Dull note heard on right upper part of chest
Auscultation-
.Normal vesicular breathsounds heard
.Decreased breath sounds on right upper lobe
.crepitations present on right mid axillary area
.vocal resonance reduced on right apical area
Cardiovascular system:
.S1 and S2 heard
.no mumurs
GIT:
.Shape of the abdomen- scaphoid
.Hernial orifices- normal
.Soft,non tender,no organomegaly
.Bowel sounds- heard
Central nervous system :
.Speech- normal
.cranial nerves- normal
.Motor system- normal
.Sensory system- normal
.Reflexes-normal
.Gait- normal
Provisional diagnosis:
Right lung upperlobe fibrosis
Investigations—
Complete blood picture:
Complete urine examination:
LFT:
AFB culture:
No acid fast bacilli
Electrocardiogram:
No regional wall motion abnormality
Ejection fraction :-67
Mild diastolic dysfunction present
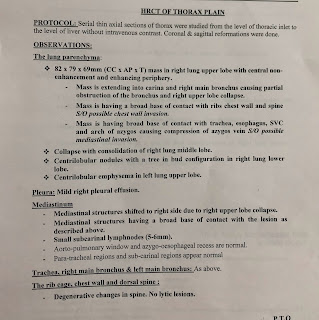
HRCT:
RFT-
.Urea-31 mg/ dl
.Creatinine-0.9
.Uric acid-3.1
.calcium- 10
.phospate-3.3
.sodium-128
.chlorine-95
.potassium-4.2
ABG-
.pH-7.44
.pCO2-34.3
.pO2 -68.3
.HCO3-23.4
.Needle thoracocentasis was done on 5 th June,2022.
.Under ultrasound guidance
.Fluid aspirated was 20 ml
.Straw coloured
Final diagnosis-
Right lung upperlobe fibrosis
Treatment-
1).Inj.augmentin-1.2 gm IV TID
2).Inj.pantop-40 mg OD
3).Tab.paracetomol-650 mg BD
4).syp.Ascoril-2 Tbsp
5).Nebulization with .budecort-BD
.Duolin-TID
.Mucomol-TID
6).oxygen inhalation with Nasal prongs@2.4 lit/ min
7).Tab.Azee-500 mg OD
02/06/2022-
O/E - patient is conscious, coherent, cooperative.
BP-120/80 mmHg
PR- 102 bpm
RR-26 com
SpO2-90% on RA
98% on 2 lit oxygen
Respiratory system examination-
Crepitations- right midaxillary area
Decreased breath sounds on right side upper lobe
Treatment-
1).Inj.augmentin-1.2 gm IV TID
2).Inj.pantop-40 mg OD
3).Tab.paracetomol-650 mg BD
4).syp.Ascoril-2 Tbsp
5)Nebulization with .budecort-BD
.Duolin-TID
.Mucomol-TID
6).oxygen inhalation with Nasal prongs@2.4 lit/ min
7).Tab.Azee-500 mg OD
03/06/2022-
O/E - patient is conscious, coherent, cooperative.
BP-120/80 mmHg
PR- 89 bpm
RR-26 com
SpO2-96% on RA
Respiratory system examination-
Crepitations- right midaxillary area
Decreased breath sounds on right side upper lobe
Treatment-
1).Inj.augmentin-1.2 gm IV TID
2).Inj.pantop-40 mg OD
3).Tab.paracetomol-650 mg BD
4).syp.Ascoril-2 Tbsp
5).Nebulization with .budecort-BD
.Duolin-TID
.Mucomol-TID
6).oxygen inhalation with Nasal prongs@2.4 lit/ min
7).Tab.Azee-500 mg OD
8)syp.Cremaffin-1ml HS
04/06/2022-
O/E - patient is conscious, coherent, cooperative.
Temperature-98.7°F
BP-120/80 mmHg
PR- 94 bpm
RR-14 com
SpO2-92% on RA
96% on 2 litres oxygen
Respiratory system examination-
Bilateral air entry- present
No added sounds
Treatment-
1).Inj.augmentin-1.2 gm IV TID
2).Inj.pantop-40 mg OD
3).Tab.paracetomol-650 mg BD
4).syp.Ascoril-2 Tbsp
5).Nebulization with .budecort-BD
.Duolin-TID
.Mucomol-TID
6).oxygen inhalation with Nasal prongs@2.4 lit/ min
7).Tab.Azee-500 mg OD
8).syp.Cremaffin-1ml HS
9).Tab.Aceclofenac-BD
05/06/2022-
O/E - patient is conscious, coherent, cooperative.
BP-120/80 mmHg
PR- 90 bpm
RR-24 com
SpO2-96% on RA
Respiratory system examination-
Bilateral air entry- normal
No added sounds
Treatment-
1).Inj.augmentin-1.2 gm IV TID
2).Inj.pantop-40 mg OD
3).Tab.paracetomol-650 mg BD
4).syp.Ascoril-2 Tbsp
5).Nebulization with .budecort-BD
.Duolin-TID
.Mucomol-TID
6).oxygen inhalation with Nasal prongs@2.4 lit/ min
7).Tab.Azee-500 mg OD
8).syp.Cremaffin-1ml HS
9).Tab.Aceclofenac-BD
10).Inj.optineurin-1 ampule
06/06/2022-
O/E - patient is conscious, coherent, cooperative.
BP-120/80 mmHg
PR- 88 bpm
RR-22com
SpO2-98% on RA
Respiratory system examination-
Bilateral air entry- normal
No added sounds
Treatment-
1).Inj.augmentin-1.2 gm IV TID
2).Inj.pantop-40 mg OD
3).Tab.paracetomol-650 mg BD
4).syp.Ascoril-2 Tbsp
5).Nebulization with .budecort-BD
.Duolin-TID
.Mucomol-TID
6).oxygen inhalation with Nasal prongs@2.4 lit/ min
7).Tab.Azee-500 mg OD
8).syp.Cremaffin-1ml HS
9).Tab.Aceclofenac-BD
10).Inj.optineurin-1 ampule
11).Diclofenac patch
07/06/2022-
O/E - patient is conscious, coherent, cooperative.
BP-120/80 mmHg
PR- 88 bpm
RR-22com
SpO2-98% on RA
Respiratory system examination-
Bilateral air entry- normal
No added sounds
Treatment-
1).Inj.augmentin-1.2 gm IV TID
2).Inj.pantop-40 mg OD
3).Tab.paracetomol-650 mg BD
4).syp.Ascoril-2 Tbsp
5).Nebulization with .budecort-BD
.Duolin-TID
.Mucomol-TID
6).oxygen inhalation at 2.4lit/min













Comments
Post a Comment